When you discover a small patch of hair loss and flaky skin on your beloved pet, your first reaction is likely, "Oh no, is it allergies again?" You might start mentally retracing their recent diet, their environment, or even switch your household cleaning products. However, while you're stuck in the "anti-allergy" mindset, a truly cunning "great pretender" may be quietly expanding its territory, not only threatening your pet's health but potentially affecting you and your family as well.
This "great pretender" is Dermatophytosis, which we commonly call "ringworm." It is dangerous not only because it is easily misdiagnosed, but also because it is a highly contagious zoonotic disease.
Today, we will take a deep dive into this topic, revealing the true nature of ringworm, analyzing its similarities and differences with allergy symptoms, and providing a scientific strategy for diagnosis and response to help you find the right path through the fog of the "itch of the century."
dermatophytosis dog cat, ringworm in cats, ringworm vs allergies in dogs, misdiagnosed ringworm, Wood's lamp for ringworm, DTM fungal culture, zoonotic skin diseases, how to clean house after ringworm, itraconazole for cats
Unmasking Ringworm: It's Not a Worm, It's a Fungus
First, we must debunk a fundamental misconception: despite its name, "ringworm" has nothing to do with any kind of worm.
-
Scientific Definition: Dermatophytosis is a superficial infection of the keratinized layers of the skin, hair, and claws caused by a group of "keratin-loving" fungi. They feed on keratin (the primary protein that makes up hair and the outer layer of skin), and in the process, they destroy the hair shaft structure, leading to hair loss and scaling.
-
Common Culprits: The most common pathogens include Microsporum canis (responsible for about 70% of feline and 40% of canine ringworm cases), Microsporum gypseum (often contracted from soil), and Trichophyton mentagrophytes (often contracted from rodents).
-
The Most Important Characteristic: Zoonotic Potential
-
Source: The U.S. Centers for Disease Control and Prevention (CDC).
-
Core Argument: In its guidelines on healthy pets, the CDC explicitly lists dermatophytosis as a significant zoonotic disease. Fungal spores can be transmitted to humans through direct contact with an infected pet or indirect contact with contaminated objects (such as combs, bedding, and carpets). Children, the elderly, and immunocompromised individuals are particularly susceptible. This means that an undiagnosed pet can become a source of infection for the entire family.
-
The Diagnostic Gauntlet: Why Is It So Often Mistaken for "Allergies"?
Dermatophytosis is called "The Great Pretender" because it can present with a wide variety of clinical signs, with the most common ones being strikingly similar to allergies: hair loss, scaling, redness, and varying degrees of itching. Therefore, a scientific diagnostic process is the only way out of this "confusing maze."
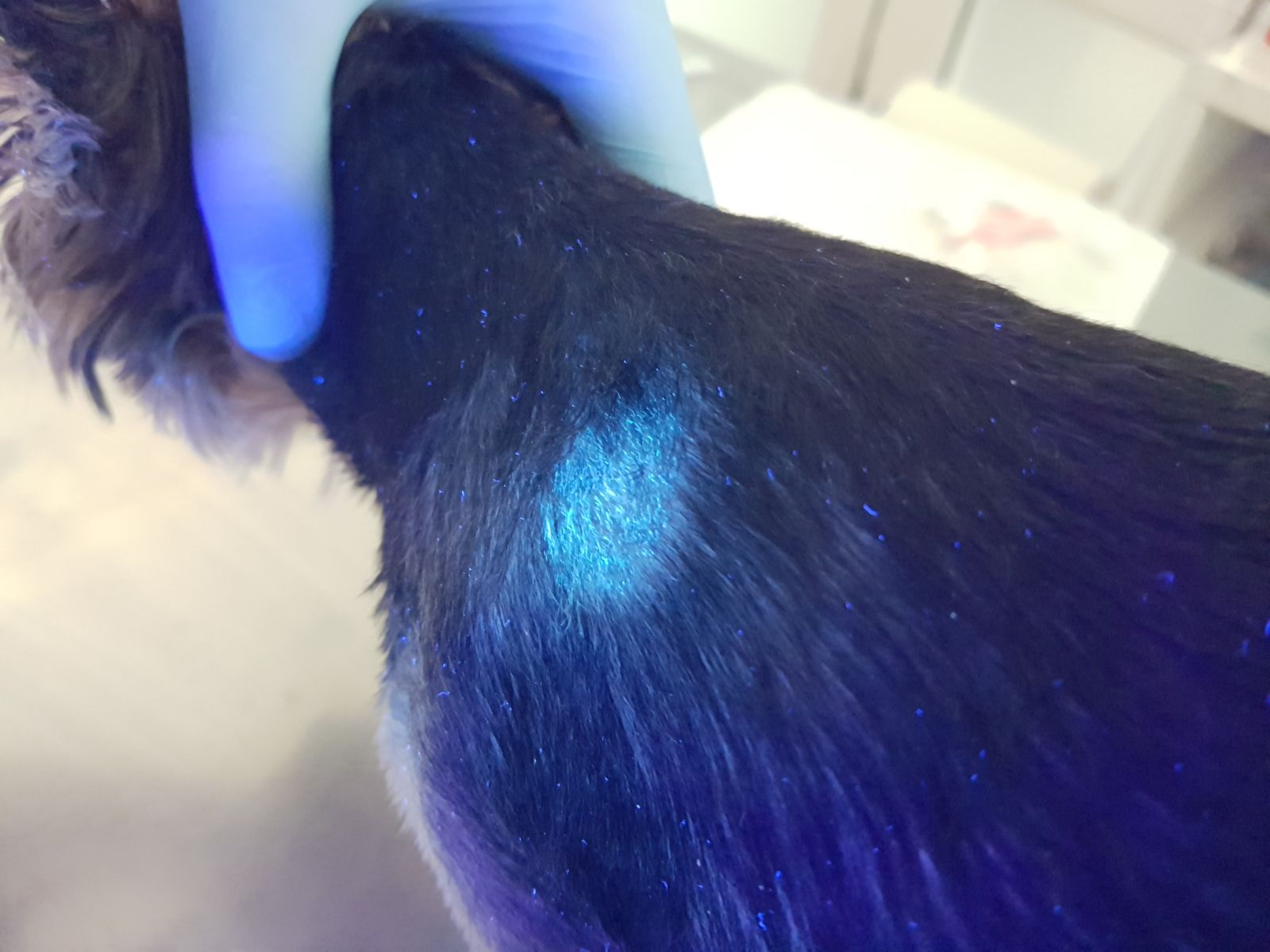
Wood's Lamp Examination: The Scientific "Searchlight" for Rapidly Identifying a "Suspect"
This is a mature and reliable rapid screening technique widely used in the professional veterinary field.
-
Scientific Principle and Advantages:
-
Sources: The application and value of this technology are jointly confirmed by multiple top-tier global veterinary institutions and authoritative literature, including:
-
The Merck Veterinary Manual
-
Clinical Practice Guidelines from the American College of Veterinary Dermatology (ACVD)
-
The Cornell Feline Health Center at Cornell University's College of Veterinary Medicine
-
Core textbooks such as Infectious Diseases of the Dog and Cat.
-
-
Core Argument: These authoritative sources, without exception, list the Wood's lamp examination as the preferred rapid screening step for suspected cases of dermatophytosis. Its scientific basis lies in its ability to use specific wavelengths of UV light to precisely identify the special metabolic byproducts of some of the most common pathogenic fungi (especially M. canis), causing them to emit a clear, unique apple-green fluorescence in the dark.
-
-
Core Value to the Owner:
-
Achieve "Day-Zero" Early Warning, Winning Golden Intervention Time: Compared to waiting for symptoms (like extensive hair loss) to become clearly visible, a Wood's lamp can sound the alarm at the earliest stage of infection, when the fungus has just begun to produce metabolites on the hair shaft. This advanced warning secures precious time for you and your vet to take action.
-
Safeguard Family Public Health, Blocking Zoonotic Risk:
-
Scientific Basis: Ringworm is a zoonotic disease recognized by the CDC that can be transmitted from pets to people. A Wood's lamp helps you establish a "biosecurity line of defense" at home, sounding the alarm before fungal spores can spread widely and threaten family members (especially children).
-
-
Reduce Potential Treatment Costs, Preventing a Minor Issue from Becoming a Major Problem:
-
Scientific Basis: The cost of treating dermatophytosis is directly proportional to the extent of the infection and environmental contamination. A localized, early-stage lesion may only require topical therapy and a short course of oral medication. In contrast, a delayed case with a systemic infection and heavy environmental contamination often requires months of expensive oral drugs and an extremely time-consuming, even professionally-assisted, complete environmental decontamination. Early detection is the most direct way to save money.
-
-
Enhance Pet Welfare, Shortening the Painful Treatment Period:
-
Scientific Basis: According to Fear Free® animal care principles, any action that prolongs a pet's discomfort or restricts its freedom increases its levels of "Fear, Anxiety & Stress" (FAS). A quicker diagnosis and earlier treatment significantly shorten the time a pet must endure itching, wear an E-collar, or be isolated, which is crucial for maintaining its mental health and quality of life.
-
-
Provide Data-Driven Peace of Mind, Turning from Passive to Proactive: Regular Wood's lamp checks transform you from passively guessing "does my pet's skin look okay?" to proactively monitoring with "I just checked, and there's no abnormal fluorescence." This sense of security, based on "data" (albeit visual data), is far more reliable than simple observation, making you the true first line of defense for your pet's health.
-
Other Key Diagnostic Tools
-
Microscopic Examination (Trichogram): Plucking hairs from the lesion's edge for direct microscopic observation can sometimes reveal fungal spores attached to the hair shaft.
-
Fungal Culture (DTM): This is one of the most widely used "gold standards" in clinical practice, as it directly proves the presence and type of a live fungal organism.
Real-World Cases: Two Winding Roads to a Diagnosis
Case Study #1: The Long-Haired Persian Cat Delayed by an "Allergy" Diagnosis
-
Case Source: A lengthy help post from a user on Reddit's r/AskVet subreddit.
-
Time & People: Autumn 2024, an owner and her 4-year-old pure-white Persian cat, "Princess."
-
Problem Progression: A small patch of hair loss appeared above Princess's eye, which the owner initially dismissed. The first vet also suspected "stress or a minor allergy" and suggested monitoring. Over the next two months, the bald patch slowly grew and new ones appeared behind her ears and on her front paw. The owner tried several expensive hypoallergenic cat foods with no effect.
-
The Turning Point: The owner developed an itchy, circular red rash on her own arm. She went to a human dermatologist with photos of herself and her cat. The doctor highly suspected "ringworm" and advised her to get the cat tested for fungus immediately.
-
Veterinary Intervention & Outcome: The new vet, after hearing the full history and the zoonotic development, immediately performed a DTM culture for Princess. On day 9, the medium turned red and a typical white colony grew, confirming a Microsporum canis infection. The treatment plan included oral itraconazole and twice-weekly antifungal medicated baths. At the same time, the entire family began a months-long environmental decontamination. Six months later, after two consecutive negative cultures, Princess and her owner were finally declared cured. This case highlights that when "allergy" treatments fail and the owner also develops a rash, ringworm must be considered the primary suspect.
Case Study #2: The "Trojan Horse" from the Shelter
-
Case Source: A public health case shared by a veterinarian on a professional exchange website to alert colleagues.
-
Time & People: Spring 2025, a loving family who had just adopted a cute 2-month-old tabby kitten named "Milo" from a local shelter.
-
Problem Progression: Milo appeared perfectly healthy at the time of adoption with no skin issues. However, three weeks after he came home, the family's 5-year-old Golden Retriever, "Goldie," developed a patch of hair loss on his nose. At the same time, the owner's two children developed "red rings" on their necks and arms.
-
Veterinary Intervention & Outcome: The owner took the entire family (including the dog and the cat) to the vet clinic. The experienced veterinarian immediately suspected dermatophytosis and examined all the animals. Under the Wood's lamp, the kitten Milo's entire body showed multiple areas of faint fluorescence under his seemingly normal coat. The DTM culture confirmed that Milo was an asymptomatic carrier and the source of the infection.
-
Conclusion: The family began a long process of treating everyone and disinfecting the environment. The veterinarian emphasized in his sharing that shelters, catteries, and other high-density animal environments are high-risk areas for the spread of ringworm. For new pets, especially young animals with unknown histories, a routine fungal screening (like a DTM culture) is a highly recommended preventative medicine measure.
The "Three-Pronged Attack" for Treatment: Systemic, Topical, and Environmental
Once diagnosed, treating ringworm is a "marathon, not a sprint," requiring patience and a three-pronged attack:
-
Systemic Therapy: Oral antifungal medications (like itraconazole or terbinafine) are the core of the treatment, and the course usually lasts for several weeks or even months.
-
Topical Therapy: Weekly or twice-weekly medicated baths with shampoos containing miconazole, ketoconazole, or lime sulfur effectively reduce the number of fungal spores on the body, lowering the risk of environmental contamination.
-
Environmental Decontamination: This is the most laborious but also the most critical part to prevent recurrence and family transmission. All hard surfaces must be thoroughly cleaned with an effective disinfectant (like a 1:10 bleach solution), and all fabrics must be washed in hot water.
Conclusion: Don't Let the "Great Pretender" Deceive Your Love
Dermatophytosis perfectly illustrates the adage "seeing is not always believing." It reminds us that in matters of pet health, a scientific, rigorous diagnostic process is far more important than guesswork based on experience. When your pet shows "allergy-like" symptoms but conventional treatments are not working, please be brave enough to ask your veterinarian that crucial question: "Should we do a fungal culture to rule out this 'great pretender'?"
One simple test could save you, your pet, and your family months of trouble and distress.